Vaccinations have been proven time and time again to prevent
disease and improve health outcomes. All around the world, vaccines have been
deployed to deal with illnesses as common as the flu and as deadly as Ebola. Meningitis
is another disease for which vaccination has become a major priority. The
“kissing disease,” at it is sometimes called, has made a number of appearances
on college campuses across the United States. While incidence in the U.S.
remains quite low, at 0.3-4 cases per 100,000 persons, incidence can be as high
as 1 case per 100 persons in the “meningitis belt” of Africa, where epidemics
occur with regularity.
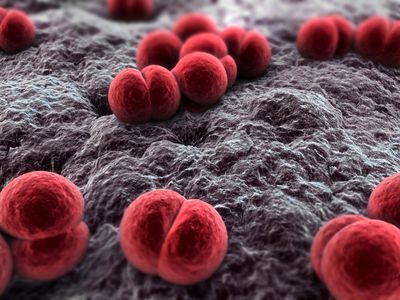 |
| Neisseria meningitidis, the bacterium responsible for meningitis. Image from Bioquell.com |
Infection with the bacterium Neisseria meningitidis, the major cause of meningitis, often goes
unnoticed. The bacteria take up residence within the nasal cavity, where they can
stay without causing disease in a carrier individual. However, in approximately
1-5% of people exposed to the bacteria, invasive disease occurs, and the
bacteria enter the bloodstream, leading to life-threatening disease.
Symptoms of meningitis typically begin almost immediately,
just one day after infection, and include flu-like symptoms of fever, headache,
and stiffness. Because the bacteria enter the bloodstream, any organ or tissue
can become infected and impaired. Despite years of research, mortality rates
continue to range from 10-15%, even in developed countries, with rates above
20% in the developing world. Even for those who survive the invasive disease
stage, meningitis causes lasting impairments in 19% of patients, with
neurological disabilities, seizures, hearing or visual loss, and cognitive
impairment being classical manifestations. The rapidity of disease progression,
along with the high mortality rate, make meningitis a prime disease target for
vaccination.
The first vaccines against meningitis were developed in the
1970s. Unfortunately, these early vaccines lacked the ability to maintain
long-lasting immunity against the bacteria. In the late 1990s, alterations were
made in the vaccine components, allowing for the elicitation of an
immunological memory response that would be effective to protect young children
into their adult years and would even help reduce the rates of carriage of the
bacteria in the nasal cavity. While this was great news for the prevention of
meningitis, challenges still remained. The bacteria that cause disease can
belong to any of 6 different serogroups, meaning that immunity to one serogroup
will not necessarily provide protection from another. This requires
differential targeting of all 6 serogroups to truly prevent disease.
 |
| Image from the Meningitis Vaccine Project |
Researchers have addressed this challenge by producing different
vaccines for use in specific parts of the world where each serogroup is
problematic. In the meningitis belt of Africa, for example, serogroup A has
historically been the cause of epidemics. To wipe out these epidemics, a mass
vaccination campaign was begun in 2010; the Meningitis Vaccine Project produced
and provided vaccines against N.
meningitidis serogroup A for over 217 million people in 17 different
countries. Thanks to these vaccines, epidemics linked to the serogroup A
bacteria have been eliminated.
Unfortunately, when one serogroup is removed, a niche opens
up for another. Just last month, the CDC announced that a small epidemic in
Liberia had been caused by the N.
meningitidis serogroup C bacteria. Nigeria and Niger have also reported
outbreaks of this serogroup. Luckily, in the case of Liberia, the country’s
response time was extremely rapid. Thanks to the health system improvements
made during the Ebola outbreak, Liberia now has a robust case detection and
monitoring system. Other countries in the area, however, are not nearly as
advanced and could suffer a severe epidemic if serogroup C moves in with force.
Great strides have been made in the fight against meningitis
outbreaks. However, the complexity of the group of bacteria responsible for the
disease leaves a number of challenges in place that must be overcome. The ideal
solution would be the introduction of a vaccine that combined pieces from each
bacteria serogroup to produce an immune response in patients that would protect
from all six serogroups at the same time. While some quadrivalent vaccines
already exist, which provide protection against four of the six serogroups,
these vaccines have only been recommended for use in the U.S. for adolescents
entering college. Protection from this vaccine only lasts 2-5 years in adults,
making it less than ideal for deployment in rural areas where boosting is not a
viable option, such as Africa. Advances in vaccine technology may help improve
the longevity of protection, making multivalent vaccination a more robust
solution to the meningitis problem. Until then, rapid case detection and
monitoring capabilities, such as those displayed in Liberia, will be the key to
keeping meningitis epidemics in check as they arise. Between vaccine and
monitoring advances, meningitis epidemics may one day become a thing of the
past.