The disease hepatitis A is caused by the hepatitis A virus (HAV). While "hepatitis" can be caused by several viruses that share similar names, the hepatitis viruses are quite different from each other. HAV is an unenveloped RNA virus from the picornavirus family, the same family as poliovirus and rhinoviruses. Alternatively, hepatitis B virus is an enveloped double-stranded DNA virus from the hepadnavirus family, hepatitis C virus is an enveloped RNA virus from the flavivirus family, and hepatitis E virus is a quasi-enveloped RNA virus currently classified in the hepevirus family (hepatitis D virus is considered a subviral satellite since it cannot replicate without the presence of hepatitis B).
 |
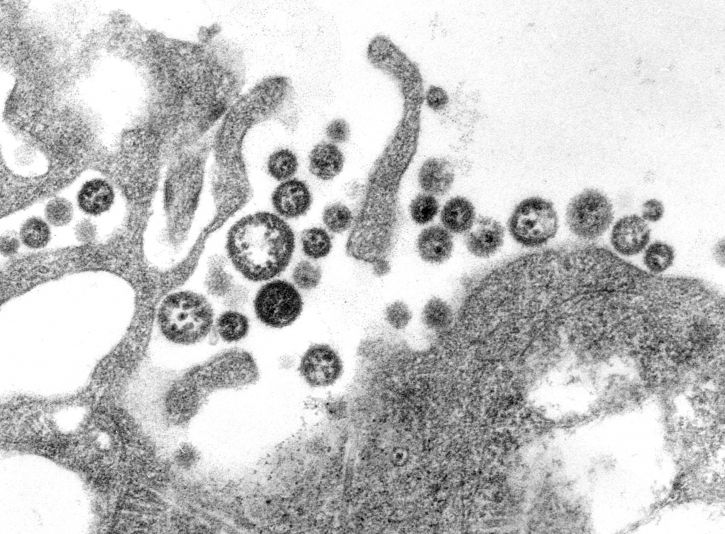
A cluster of HAV virions
CDC's Public Health Image Library.
Image # 2739; photo credit: CDC/Betty Partin.
|
A vaccine for HAV exists and is extremely effective at preventing disease. Children are routinely vaccinated around age 1, providing protective immunity against the virus. Unfortunately, the vaccine was not approved for use until 1995, so many adults over the age of 25 have never been vaccinated and remain susceptible to HAV infection. Vaccination in adults is an option but is only routinely done for high-risk individuals, such as people traveling to countries where hepatitis A is common, caring for an individual with hepatitis A, or using recreational drugs. The vaccine can be given as a prophylactic before exposure or as a treatment post-exposure; as long as a person is vaccinated within 2 weeks of exposure, infection can still be prevented. However, mobilization of the vaccine to those at highest risk of infection in these outbreaks has been difficult due to the barriers in access to health care that exist for the homeless and drug-using populations. Additionally, other than the vaccine, there is no real treatment for HAV infection; giving patients rest, fluids, and adequate nutrition is the only course of action.
While local health agencies and the Centers for Disease Control (CDC) have been working to contain these outbreaks and prevent further spread, vaccine availability and lack of funding have threatened efforts. When the outbreaks began, demand for the vaccine increased dramatically, leading to shortages in the vaccine supply. Fortunately, this issue has since been resolved thanks to vaccine suppliers GlaxoSmithKline and Merck ramping up production. However, the Section 317 Immunization Program from the CDC that has been essential in paying for these vaccines has already experienced funding cuts and may experience more in the coming year. Additionally, many public health officials feel they are not being provided with enough funding to support the other essential componenets of combating viral hepatitis.
Since the virus is spreading from person-to-person contact in these outbreaks, improved sanitation and hygiene are key to reducing spread. Achieving these goals in the populations at risk has not been an easy task. In California, officials resorted to cleaning their public buses, streets, and even sidewalks with bleach to complement their vaccine distribution campaigns. It is now believed that the outbreak in California is over, giving hope that employing similar strategies could improve outbreak containment in other states. Outside California, the number of cases per day has been trending downwards in some areas, but that trend has not been consistent, and officials warn that there is still a significant threat. Improving sanitation for the over 500,000 Americans experiencing homelessness is an essential measure to end the hepatitis A outbreaks and prevent future infectious disease outbreaks in the United States. In a tough funding climate, this will not be easy to achieve, but state health departments and private non-profits are working vigilantly towards this goal. Until then, wash your hands, wash your hands, and wash your hands to help fight the spread of HAV.
Latest case report statistics, July 2018
State
|
Cases
|
Hospitalizations
|
Deaths
|
Arkansas
|
63
|
Not reported
|
≥ 1
|
California
|
704
|
461
|
21
|
Indiana
|
298
|
136
|
1
|
Kentucky
|
1,221
|
687
|
8
|
Michigan
|
865
|
695
|
27
|
Missouri
|
145
|
63
|
0
|
Ohio
|
176
|
114
|
0
|
Tennessee
|
113
|
64
|
0
|
Utah
|
264
|
139
|
≥ 2
|
West Virginia
|
699
|
428
|
2
|
Total
|
4,548
|
≥ 2,787
|
≥ 62
|